
200 years ago, the average lifespan was 35. Today it’s 73 to 79. This dramatic increase in life expectancy is a direct result of advancements in medical science. From vaccines that prevent viral outbreaks to treatments for chronic and incurable illnesses that extend life expectancy, as technology improves so does healthcare.
However, as longevity increases so do the demands placed on healthcare systems. Estimates predict that by 2050, one in four people in Europe and North America will be over the age of 65. This will put additional pressure on an already burnt-out workforce, and is expected to impact costs, patient wait times, and quality of care.
And the industry is already struggling to keep up. The World Health Organization (WHO) estimates that by 2030, we’ll experience a global shortage of healthcare professionals — in the range of 18 million. So, the trillion-dollar question is, “How can healthcare systems continue to grow exponentially without risking patient or employee safety?”
Two words: Artificial intelligence.
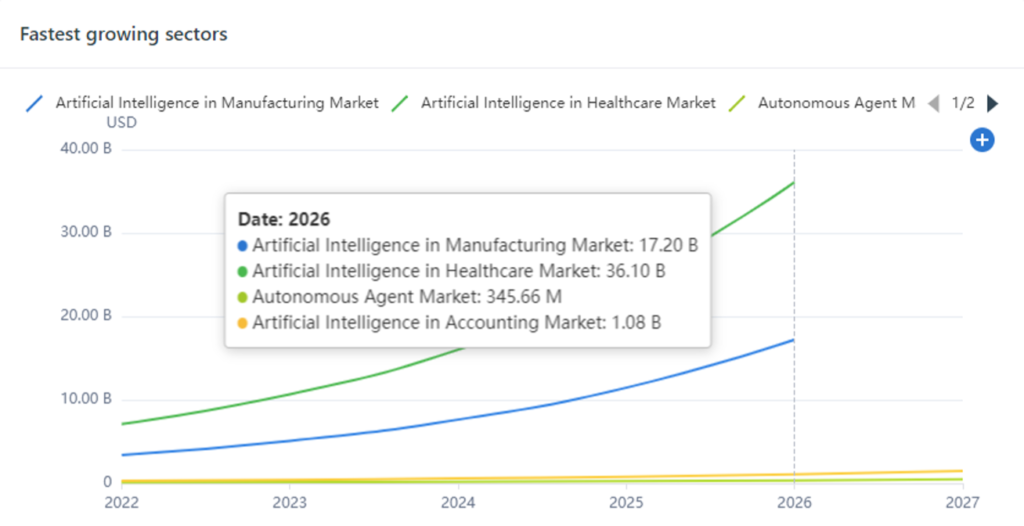
As the chart above illustrates, artificial intelligence (AI) in healthcare is the fastest-growing sector in the AI market. This isn’t surprising, given AI improves diagnostics, treatment, accuracy, outcomes, and quality of care. Plus, it enhances the day-to-day life of healthcare practitioners by automating manual tasks such as patient intake forms. As a result, doctors and nurses can spend more time looking after patients and focusing on the issues at hand.
AI in Healthcare Today
A recent OECD report found governments in Finland, Italy, Portugal, Slovenia, China, and the US are investing heavily in AI-related research initiatives. Some of these investments focus on how to evaluate the efficacy of treatments, identify medical errors, and enhance patient care.
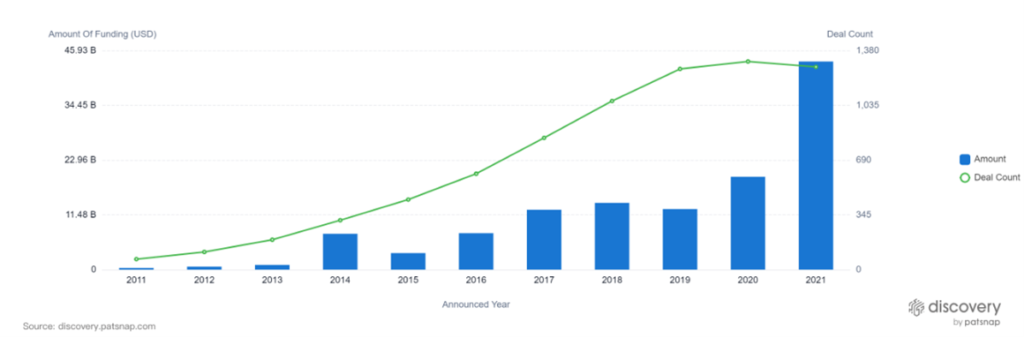
Additionally, the private sector is also playing a pivotal role. In 2021, private organizations funneled $40B into companies focusing on AI in healthcare.
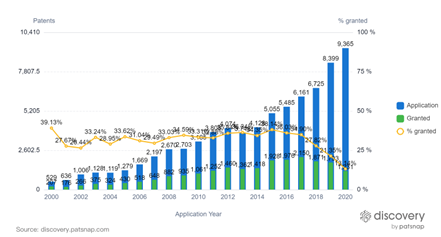
Although AI first emerged in the 1950s, patent activity didn’t take off until around 2014.* Today, AI-related inventions are booming, resulting in a dramatic shift from theory to commercial-ready technology.
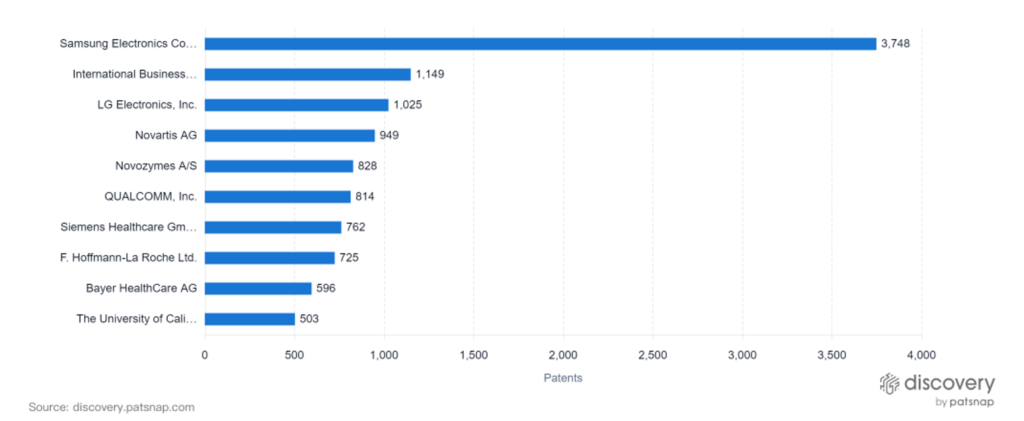
Patent data also shows the extent to which the major tech companies are the top innovators in the healthcare AI space, not the healthcare companies. As tech companies have expertise in AI, cloud, data management, and AI already, these organizations can deliver game-changing solutions to the healthcare market.
The graph below highlights key patent filers in the space. Unsurprisingly, Samsung, IBM, and LG Electronics own the top three positions.
Although AI is poised to disrupt healthcare as we know it, offering countless benefits in patient care and efficiency, there are innate challenges as well. In the following section, we’ll explore the pros and cons of AI in healthcare.
Benefits of AI in Healthcare
AI’s impact on the workforce will be more than just jobs lost or gained — the world itself will change. Its implementation will truly improve patient care. Beyond just administrative efficiency improvements, it can augment a range of clinical activities and help practitioners access information leading to better patient outcomes and quality of care. This will increase the speed and accuracy of diagnostics, providing practitioners with accurate, real-time data. Plus, it enables remote patient monitoring which empowers people to take proactive self-care measures.
Additionally, it will disrupt healthcare education. Instead of needing to memorize and regurgitate information, healthcare professionals will be able to focus on continuous learning and improvement, providing a better patient experience.
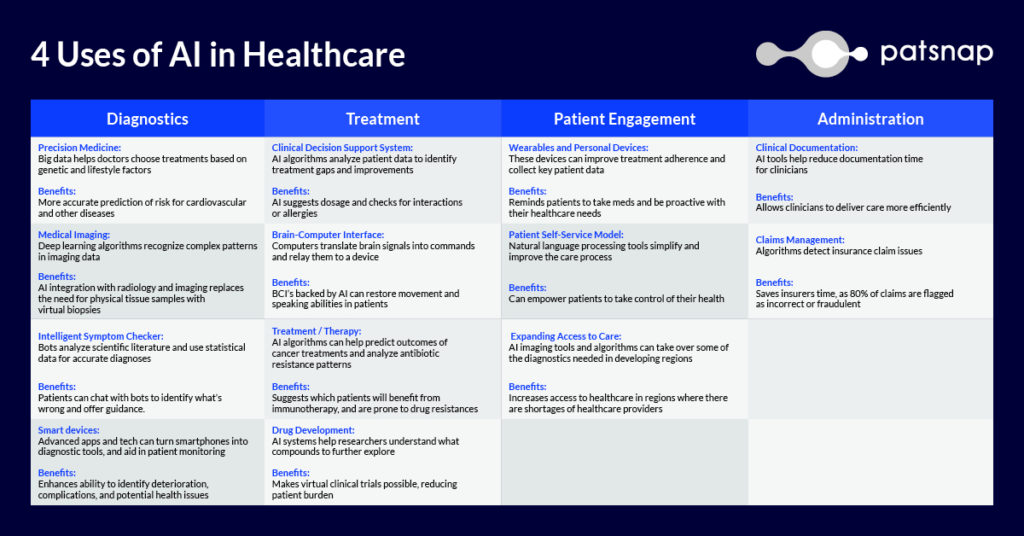
4 Uses of AI in Healthcare
Drawbacks of AI in Healthcare
Despite the potential AI offers, it may also bring considerable threats to privacy, ethical concerns, and potential for medical errors. To balance the risks and rewards of AI in healthcare, collaboration among tech developers, regulators, end users, and consumers is essential
Privacy and Security
AI presents a new set of challenges related to data privacy and security, and these issues are compounded by the fact that most AI algorithms need massive datasets for training and validation. Storing large datasets in a single location — no matter how seemingly secure — increases cyber security risks. As such, regulations related to how patient data is protected in AI-powered technologies is essential.
However, AI falls into a regulatory gray area, meaning it’s difficult to ensure patient privacy is upheld. In addition to traditional privacy concerns and cyber hacking, a study by the University of Pittsburg in 2021 found that cyberattacks using falsified medical images could fool AI models. This study shed light on the potential concept of adversarial cyberattacks in which hackers aim to alter images or data points to make AI models draw false conclusions, resulting potentially dire consequences for patients.
Ethics, Responsibility and Oversight
In terms of ethical responsibility as it relates to AI, many debates center around who’s to blame if there’s a life-altering mistake.
In March of 2018, a self-driving Uber killed a pedestrian in Arizona; the car’s programming only recognized pedestrians at crosswalks, not when crossing in the middle of the street. While this seems like a simple situation that is easy to predict, healthcare has so many situations where human behavior is hard to predict.
For example, if AI makes a mistake in interpreting radiological scans, matching drugs with disease states, or assigning hospital beds, an unknown number of patients could be at risk before any problems are detected, traced or corrected. In this instance, whether these errors affect a handful of patients or hundreds of patients, where will those affected direct their anger and grief? The computer? The doctor? The hospital managing the computer?
These are the issues that must be identified and solved ahead of time. Additionally, AI is presumed to be free of social and experiential bias. However, the algorithms may be more susceptible than people when it comes to making assumptions. This is especially true if the data the AI is trained on is incomplete or skewed towards one perspective or another.
In 2021, the WHO released the first global report on the ethics and governance of AI in healthcare, where the organization emphasized the potential disparities that could emerge with the implementation of AI, particularly because many AI algorithms are trained on data collected from patients in high-income care settings. The WHO also mentioned that ethical factors should be considered during the design, development, and deployment of AI technology.
Those working on AI should operate under the following ethical themes:
- Protecting human anatomy
- Promoting human well-being and safety and the public interest
- Ensuring transparency, explainability, and intelligibility
- Fostering responsibility and accountability
- Ensuring inclusiveness and equity
- Promoting AI that is responsive and sustainable
To successfully merge AI with healthcare, ethical considerations, accuracy, and safety must be the top priorities.
Conclusion
In the years to come, we expect AI to revolutionize healthcare. With limitless potential, AI is poised to improve diagnosis, treatment, research, and patient care. However, to unlock its full potential, patient safety and security must be the number one priority.
